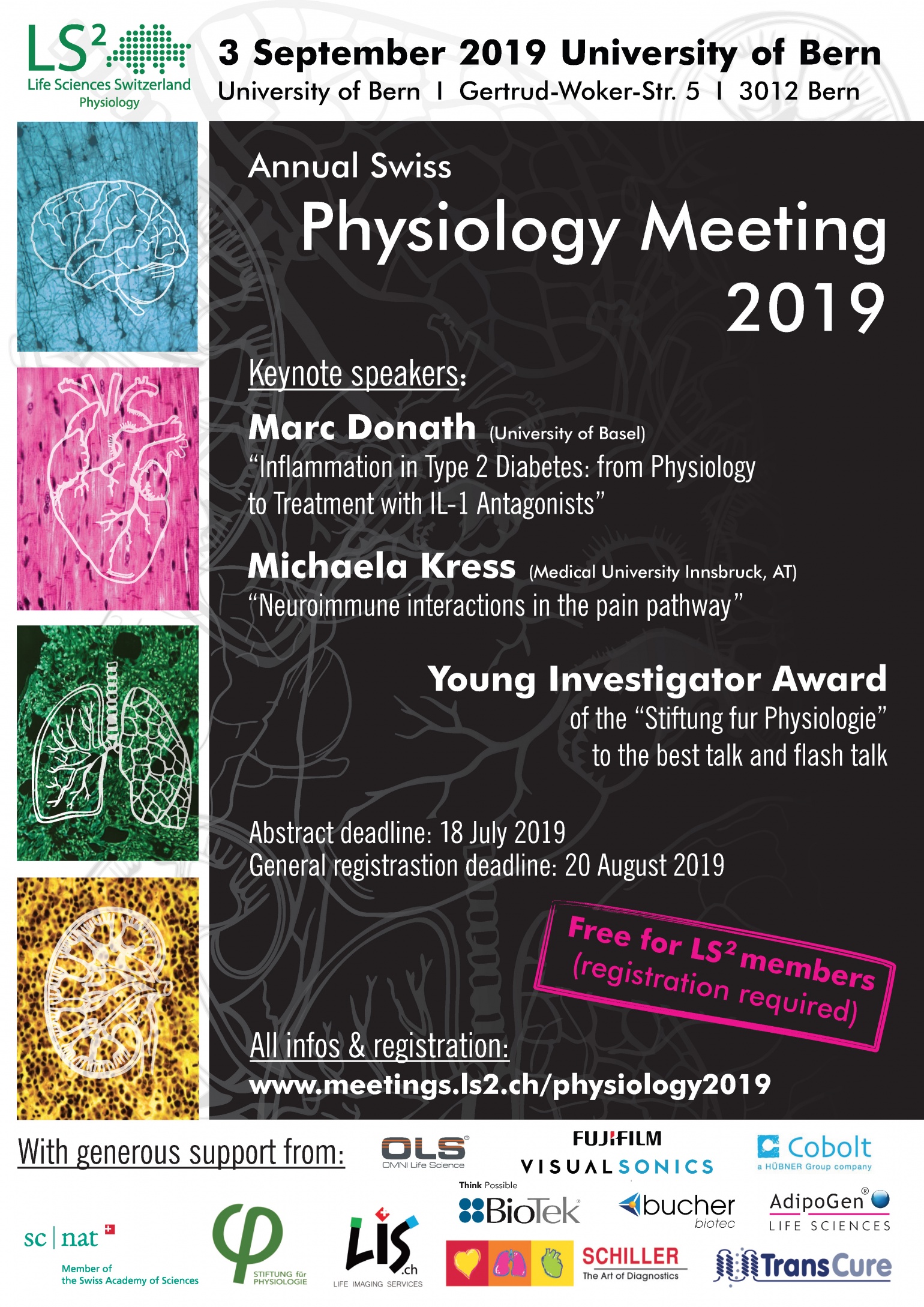
Prof. Marc Donath (University of Basel)
"Our research focuses on the mechanisms and therapy of insulin production by the pancreatic islets in physiology and in obesity associated type 2 diabetes. Our ongoing studies aim at understanding the physiological role of the immune system in metabolism. The general objective is to uncover mechanisms on how the innate immune system contributes to the adaption of pancreatic islet function under various physiological (postprandial and pregnancy) and stressful (obesity and diabetes) situations with a focus on macrophages derived IL-1beta in the postprandial stimulation of insulin; Beta-cell and placenta produced IL-1beta and IL-1Ra, and of alpha cell derived GLP-1 in physiology and insulitis; IL-33 induced ILC2 stimulated insulin secretion."

The title of his talk will be:
"Inflammation in Type 2 Diabetes: from Physiology to Treatment with IL-1 Antagonists" (please find the abstract below)
Morphological and therapeutic interventions have uncovered an inflammatory process in patients with type 2 diabetes. This inflammation is due to a pathological activation of the innate immune system by metabolic stress and is partly governed by IL-1 signaling. Initially, the inflammatory response is probably deployed to promote adaptation and regeneration. Indeed we identified a role for IL-1β and insulin in the regulation of both metabolism and immunity in response to feeding. Yet, as it becomes chronic, activation of auto-inflammatory processes may then become deleterious. It follows that modulation of inflammatory mediators may present as a possible causal therapy. This is supported by clinical studies showing that IL-1 antagonism decreases glycated hemoglobin. Furthermore, IL-1 antagonism prevents cardiovascular diseases, the major complication of diabetes.
Prof. Michaela Kress (Medical University Innsbruck, AT)
"The research in my group focuses on the pathogenesis of neuropathic and neurogenic pain disorders. We explore interactions between the nervous system and the immune system occurring upon nerve injury. At present we are mainly interested in proinflammatory cytokines (interleukin 6, LIF OSM), and the effects they have on neuronal function. We focus on the regulation of ion channels of the TRP family (TRPV1, TRPA1) by signals originating from immune cells including microglia and the neurons themselves. As novel players, non-coding RNAs and their suitability as disease biomarkers or treatment strategies are assessed."

The title of her talk* will be:
"Neuroimmune interactions in the pain pathway" (please find the abstract below)
Primary nociceptive afferents are sensors of immune signals which cause nociceptor excitation and sensitisation giving rise to ongoing pain sensation or hypersensitivity to mechanical or thermal stimuli. In particular, the pleiotropic interleukin-6 like cytokines act on nociceptors via neuronally expressed glycoprotein 130 signal transducer (gp130st) subunits and contribute to the generation of heat and mechanical hypersensitivity in mouse models of inflammatory, neuropathic and cancer pain. Cytokines acting via gp130st regulate TRPV1 and TRPA1 ion channels and in addition via neuronal signals impact on neuroinflammatory signatures such as spinal microgliosis and immune cells invading into inflamed tissue or the dorsal root ganglion. Together, our data support the conclusion, that neuroimmune interactions not only regulate nociceptor function but also seems to be critically involved in the control of the immune reaction to injury by sensory neurons.
*Sponsored by the NCCR TransCure gender equality program