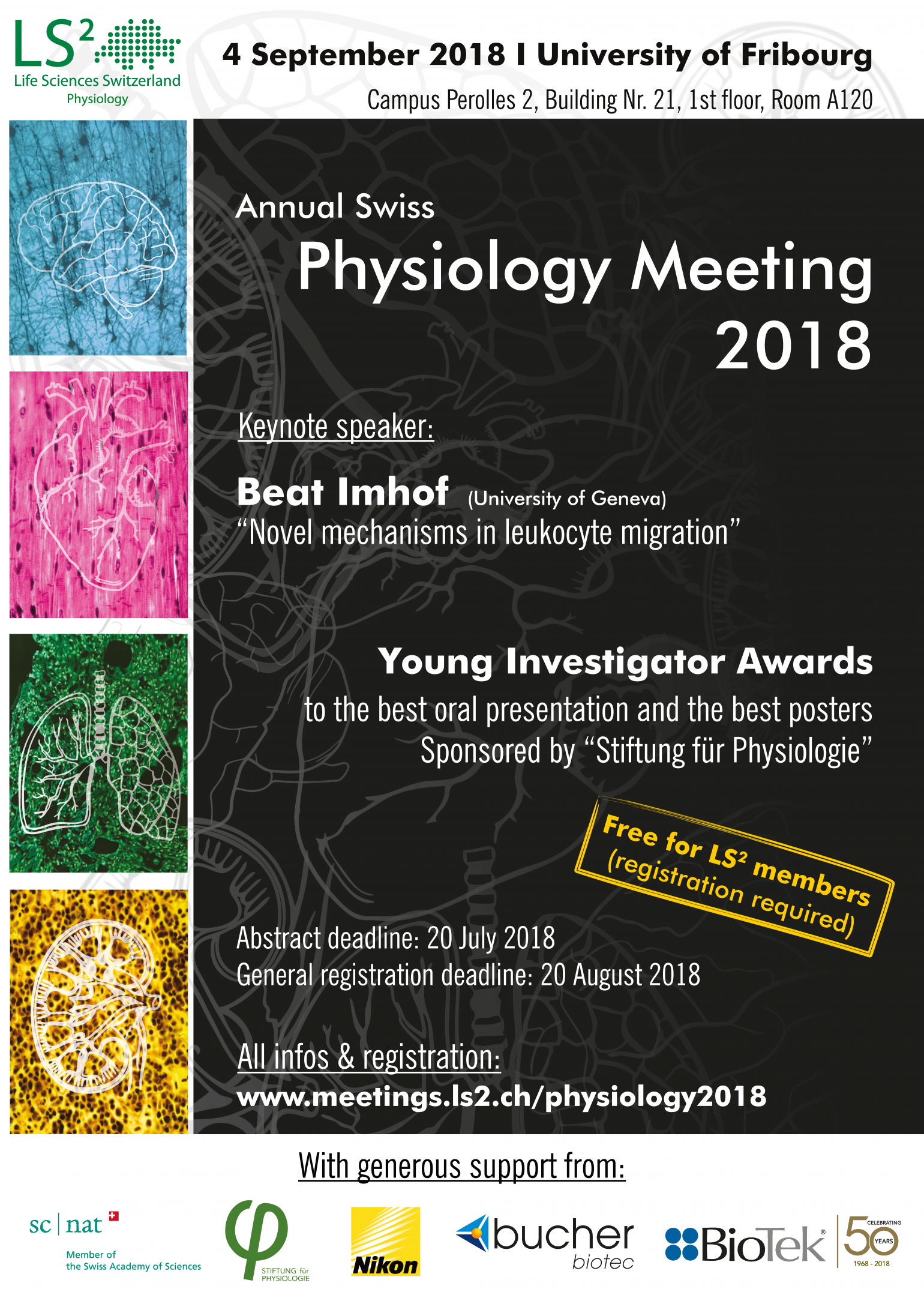
We're extremely happy that Prof. Beat Imhof (University of Geneva, currently on sabbatical in Turku/Finland) will be the plenary speaker of this year's Physiology Meeting!
The title of his talk will be: "Novel mechanisms in leukocyte migration" (Please find the abstract below)

Beat A. Imhof is a honorary professor at the Medical Faculty, University of Geneva, Switzerland and was chair of the Department of Pathology and Immunology for more than 10 years. He is part of many professional societies and was president of the Swiss Society for Allergology and Immunology (SSAI)and the European Society for microcirculation (ESM). He is editor of scientific journals and serves in numerous advisory boards. He studied Biochemistry in Zurich, Switzerland, did then his PhD at the Friedrich Miescher Laboratory of the Max Planck Institute in Tübingen, Germany (1983) where he studied cell-cell contacts. He moved as an EMBO fellow to Paris at Institute of Embryology where he worked on thymus homing of T-cell progenitor cells. In 1988 he joined the Basel Institute for Immunology, Switzerland, where he continued to study the migration of pro-T cells to the thymus. In 1997, he accepted a position as Professor for Experimental Pathology at the Medical Faculty of the University of Geneva. He there investigated the pathology of leukocyte migration in inflammatory diseases and tumor angiogenesis. His research led to many patent applications in the domain of tumor angiogenesis and therapeutic antibodies. Prof. Imhof was organizer of many scientific congresses and meetings with international participation. He is now on sabbatical leave at Turku University, Finland.
imhof-b-abstract.pdfAbstract: Beat Imhof
Inflammation is characterized by the recruitment of leukocytes from the bloodstream. In mice, the rapid arrival of neutrophils is followed by a wave of inflammatory lymphocyte antigen 6 complex (Ly6C)-positive monocytes. In contrast Ly6Clow monocytes survey the endothelium in the steady state, but their role in inflammation is still unclear. Using confocal intravital microscopy, we showed that upon viral Toll-like receptor 7/8 (TLR7/8)-mediated inflammation of mesenteric veins, platelet activation drives the rapid mobilization of Ly6Clow monocytes to the luminal side of the endothelium. After repeatedly interacting with platelets, Ly6Clow monocytes commit to a meticulous patrolling of the endothelial wall and orchestrate the subsequent arrival and extravasation of neutrophils through the production of proinflammatory cytokines and chemokines. At a molecular level, we showed that cysteine-rich protein 61 (CYR61)/CYR61 connective tissue growth factor nephroblastoma overexpressed 1 (CCN1) protein is released by activated platelets and enables the recruitment of Ly6Clow monocytes upon vascular inflammation. In addition endothelium-bound CCN1 sustains the adequate patrolling of Ly6Clow monocytes both in the steady state and under inflammatory conditions. Blocking CCN1 or platelets with specific antibodies impaired the early arrival of Ly6Clow monocytes and abolished the recruitment of neutrophils. These results refined the leukocyte recruitment cascade model by introducing endothelium-bound CCN1 as an inflammation mediator and by demonstrating a role for platelets and patrolling Ly6Clow monocytes in acute vascular inflammation.
Monocyte diversity found in human also leads to complex roles in chronic inflammation and tumor physiopathology. We now have characterized human, non-classical CD14dimCD16+ patrolling monocytes as a proangiogenic subset supporting tumor growth. These monocytes were captured by the tumor vasculature stimulated by IFNg or TNFa. They induced the chemokine CX3CL1 and led to continuous crawling of the proangiogenic monocytes along the endothelium, thus hampering extravasation. Transendothelial migration was initiated by simultaneous exhibition of cytokines and tumor derived angiogenic factors including VEGF. The recruited proangiogenic monocytes further boosted angiogenesis by secreting MMP-9, leading to release of more matrix bound VEGF. This cascade amplified the entry of angiogenic monocytes to the tumor and chronically inflamed tissue. This sets the stage for combined therapies with anti-angiogenic and IFNg-based immunotherapy for solid tumors. In summary, we have defined new mechanisms that explain acute and chronic inflammation, the latter also applies to tumors.